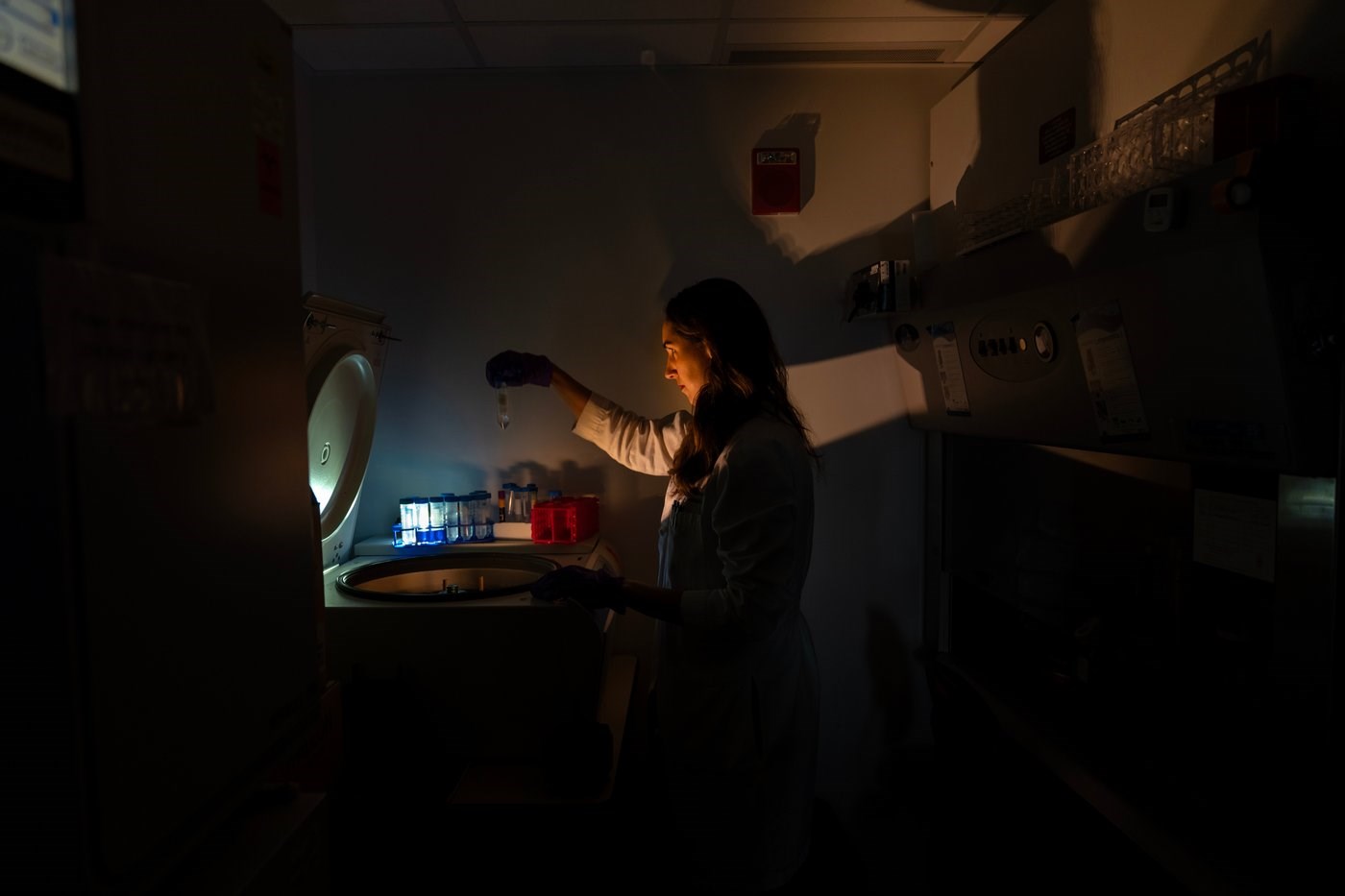
Dr. Laura Lewandowski, a pediatric rheumatologist and assistant clinical investigator, poses for a portrait at a centrifuge with tubes containing patient samples for autoimmunity testing in the lab where she works at the National Institutes of Health, Monday, Aug. 25, 2025, in Bethesda, Md. Lewandowski leads a team studying the genetics of pediatric lupus. "I've always been a person who loves puzzles and problem solving and the big picture of how people get sick. What I'm explaining to my family is that I'm a gene hunter. I could do back flips, inside that's how I feel when I can see something new. It's amazing. What I am studying, I feel it's a super exciting moment to be doing this." (AP Photo/David Goldman)
November 13, 2025 - 1:08 AM
A peek inside some leading research labs shows how scientists-turned-detectives are painstakingly decoding what causes autoimmune diseases and how to stop the immune system from attacking you instead of protecting you.
It’s a huge challenge. By the National Institutes of Health’s newest count there are about 140 autoimmune diseases affecting tens of millions of people.
Unraveling them requires patience, persistence — and sophisticated technology to even see the suspects. Researchers use laser-powered machinery and brightly colored fluorescent dyes to tell rogue cells from normal ones.
Take Type 1 diabetes, caused when cells in the pancreas that produce insulin are gradually killed off by rogue T cells. In a biomedical engineering lab at Johns Hopkins University, researchers examine mouse pancreas cells on a computer screen. Red marks the killer cells. In yellow are “peacemaker” cells that are supposed to tamp down autoimmune reactions – but they’re outnumbered.
Another type of immune cell, B cells, drive autoimmune diseases by producing antibodies that mistake healthy tissue for foreign invaders. At NIH, Dr. Iago Pinal-Fernandez studies myositis, a poorly understood group of muscle-weakening diseases. His research shows rogue antibodies don’t just damage muscles by latching onto their surface. They can sneak inside muscle cells and disrupt their normal functions in ways that help explain varying symptoms.
“When I started, nothing was known about the type of autoimmune disease we study. Now finally we’re able to tell patients, ’You have this disease and this is the mechanism of disease,” he said.
In another NIH lab, Dr. Mariana Kaplan’s team is hunting the root causes of lupus and other autoimmune diseases — what makes the immune system run amok in the first place — and why they so often strike women.
Today's drugs tamp down symptoms but don't correct the problem. Now in early-phase clinical trials are treatments that instead aim to fix dysfunctional immune pathways.
At Hopkins, scientists are working on next-generation versions, not yet ready to try in people. In one lab, they're developing nanoparticle-based treatment to dial down pancreas-killing cells in Type 1 diabetes and ramp up “peacemaker” cells.
And in another Hopkins lab, researchers are developing what they hope will become more precise treatments for rheumatoid arthritis, lupus and other antibody-driven illnesses – drugs that search out and destroy “bad” B cells.
—-
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education and the Robert Wood Johnson Foundation. The AP is solely responsible for all content.
This is a documentary photo story curated by AP photo editors.
News from © The Associated Press, 2025