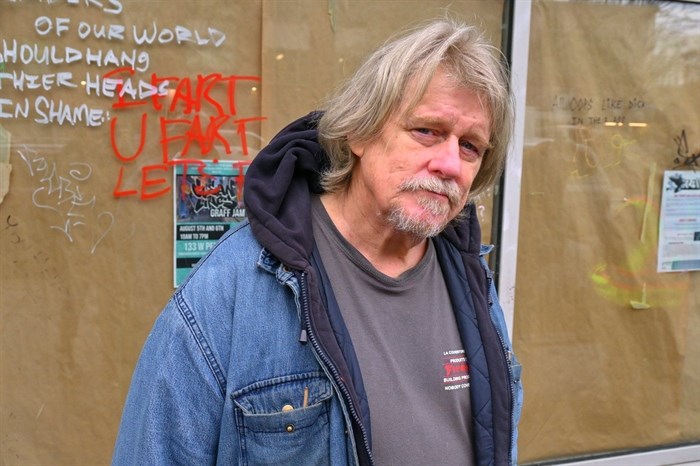
William Bernier, who was knocked out cold after unintentionally taking xylazine, says the province needs to make drug testing services far more accessible.
Image Credit: Michelle Gamage, Local Journalism Initiative
December 17, 2023 - 7:00 PM
It took only one puff of drugs cut with xylazine to knock the tall, solidly built William Bernier out for an hour.
Bernier, who didn’t know he was taking xylazine, was alarmed by the sudden powerful rush despite having more than a decade’s worth of experience using drugs. First, he felt like he couldn’t breathe. Before he knew it, he’d passed out.
When he finally came to, he was relieved to find a friend watching over him and that he hadn’t been robbed or assaulted.
But not everyone who has had a run-in with xylazine in Vancouver’s Downtown Eastside lately has been as lucky.
Xylazine, also known as tranq or tranq-dope when mixed with opioids, is a sedative approved for veterinary use in Canada as an anesthetic for animals. It is not approved for human use.
The substance has nonetheless entered the unregulated drug supply, which is alarming advocates and people who use drugs.
The provincial government says it is testing seized drugs for xylazine and that the drug’s prevalence is on the rise, though still in less than 10 per cent of seized drugs in British Columbia.
People who use drugs and live in Vancouver’s Downtown Eastside say xylazine is contributing to an increase in rates of robbery, sexual assault and infections that lead to amputations. People are also concerned the drug is making it harder to access social services and detox programs.
Xylazine is a vasoconstrictor, which means it limits blood flow to the skin. People who use xylazine can develop cuts and sores, which can become infected, and they run a higher risk of developing an infection from even a small, unrelated cut, said Dr. Alexis Crabtree, a public health physician with the BC Centre for Disease Control.
It’s not yet clear how xylazine will affect the province’s already extremely toxic unregulated drug supply, Crabtree said.
Benzodiazepines in BC’s unregulated drug supply
Unregulated drugs are currently incredibly potent and can have a dangerous or even deadly combination of other substances mixed in with them. A typical sample of unregulated opioids, simply referred to as “down,” will generally have several different opioids and benzodiazepines in it, Crabtree said.
Benzodiazepines are a large class of drugs that include regulated medications like Xanax and unregulated substances like etizolam. Benzodiazepines are generally used as sedatives and to treat short-term anxiety, Crabtree said.
It’s possible the high rate of benzodiazepines in B.C.’s unregulated supply will mean that xylazine won’t get added in large amounts as it does in eastern U.S. states, Crabtree said. However, it’s hard to predict where the unregulated drug market is headed, she added.
Benzodiazepines are highly addictive and can cause people to have seizures and even die during withdrawal, she said. Xylazine isn’t necessarily addictive but a person can get used to taking it and then experience symptoms when they stop taking it. This is similar to, for example, when a person stops taking antidepressants, which are not addictive but can cause hallucinations when stopped cold turkey, she said.
Combining opioids with benzodiazepines makes the opioids have a stronger effect on the body, Crabtree said. This means people can overdose easier because the benzodiazepines increase how much an opioid reduces a person’s breathing.
Unregulated drug deaths involving benzodiazepines have been on the rise in B.C. since 2018 when they were involved in roughly three per cent of overdose deaths. In 2022, the latest year of reported data, they were involved in over 29 per cent of overdose deaths, according to the BC Coroners Service.
The BC Centre on Substance Use’s drug checking results website says 16 per cent of the drugs tested in B.C. contain benzodiazepines.
The effects of xylazine
Then there’s xylazine. The drug drops blood pressure, relaxes muscles and makes people sleepy or sedated, Crabtree said. Xylazine can also make the effects of opioids last longer and can help treat some symptoms of opioid withdrawal, like restlessness and discomfort, she added.
A Toward the Heart resource on xylazine says the drug increases the risk of overdosing on other depressants, such as alcohol, benzodiazepines and fentanyl.
Xylazine makes its way through your body quickly and takes around 45 minutes before the effects begin to decline, said Aaron Shapiro, associate scientific director of toxicology at the BCCDC.
Clinical toxicology tests can confirm whether a person took xylazine within the last 24 hours, and a post-mortem toxicology test can confirm if a person took xylazine within three hours before they died, Shapiro said.
The Tyee spoke with several people who use drugs and live in the Downtown Eastside, who said they’d unintentionally used xylazine or had friends who had.
One man who spoke with The Tyee said that when he injected a substance that contained xylazine, he was knocked out before he could take the needle out of his arm.
Gary Davison, community liaison and harm reduction program manager for the Heart Tattoo Society, said he’s seen an increase in burns on people’s faces, hands and torsos because they will use a torch lighter to smoke a drug with xylazine in it and pass out before they can turn the torch off. People also have scrapes on their foreheads and chins because they will pass out and fall forward, he said.
Les Kaczorowski, a Coalition of Peers board member, said he woke up after unintentionally taking xylazine to find that all of his possessions except one shoe had been stolen.
Two people spoke of how xylazine has impacted their friends. One person said their friend had lost count of the number of times she had been sexually assaulted after taking xylazine. Another lost a steady job as a longshoreman after xylazine made them miss several shifts.
More xylazine enters the unregulated market
Xylazine’s prevalence is on the rise. In January 2020, 1.4 per cent of unregulated fentanyl seized by law enforcement and tested by Health Canada had xylazine mixed in, Crabtree said. By April 2023 that number had increased to nine per cent. Substance Drug Checking, a testing service run by the University of Victoria, found less than five per cent of opioid samples contained xylazine.
Crabtree said it’s not possible to know why drug dealers cut other substances into their drugs but it could have something to do with how xylazine, like benzodiazepines, makes the effects of opioids stronger.
Davison said xylazine is being added to unregulated drugs because it is cheap (he calculates it to be worth $10 per kilogram), can bulk out a substance, is readily available in Canada and can make small amounts of opioids feel stronger.
Xylazine isn’t designated for human use because of how it can create skin ulcers and increase the risk that a puncture mark from a needle or even a small unrelated scratch can get infected, Crabtree said.
In Pennsylvania, xylazine is found in 90 per cent of unregulated opioids and is leading to a spike in overdose deaths, infections and amputations. In response, the state’s governor is asking the country to more tightly regulate xylazine.
It’s important to remember that there are a lot of social determinants of health that play into a person’s ability to fight off an infection, Crabtree said. Not everyone with a cut, sore or amputation is necessarily using drugs. If a person is unhoused, it may be harder for them to keep a bandage clean and dry and get lots of sleep and rest to help fight off an infection, she said.
Even though he’s cautious, Coalition of Peers’ Kaczorowski said he’s unintentionally used tranq-dope twice and worries it may be the reason an infection has swollen his right leg.
Xylazine can also complicate overdose treatment. An opioid overdose can be temporarily reversed by administering naloxone, but xylazine and benzodiazepines don’t respond to naloxone.
“A person may have their breathing restored to normal by naloxone but they could still be very sedated and won’t necessarily wake up all the way,” Crabtree said. That sedation can hide other medical problems, which makes it challenging for health-care workers to know how to respond, she said.
Because xylazine affects people for such a short amount of time, Davison said, he’s worried people’s mobility will be limited as they spend their days in short cycles of being affected by the drug and then seeking it back out when it’s left their system. This reduces their ability to access social and medical services, like parole and wound care, he said.
This fear was echoed by people who use drugs.
Kaczorowski said that while he regularly tests the drugs he sells and uses, “no one is going to walk five blocks to get their drugs tested when using tranq-dope.”
Davison said this is why the B.C. government and health authorities need to change their health-care approach and develop mobile clinics where teams of doctors, nurses, peer support staff and social workers can walk out into the community and meet people on sidewalks, in alleys or in parks to help with wound care or antibiotic treatment, or to connect with services as needed.
Minister of Mental Health and Addictions Jennifer Whiteside told The Tyee it is “critical” to build out more access to primary care.
“We want to keep people alive to get them into care and build relationships with people who need them and provide them with access to the supports they need,” she said.
It’s possible to create mobile health-care teams too, she said, noting how Vancouver Coastal Health launched a mobile team to support Indigenous women earlier this year.
Right now the province is not looking to add more mobile vans, she added.
Davison said benzodiazepines and xylazine are also complicating the detox process because people have more complex care needs, like wound care, when trying to get off these drugs.
Vancouver Coastal Health told The Tyee benzodiazepines require a medical detox model with 24-hour monitoring and that “we are seeing more of these complicated withdrawal cases at our detox facilities since benzodiazepines became more prevalent in the unregulated drug supply.”
However, Vancouver Detox is able to “fully support” people withdrawing from benzodiazepines and other substances including xylazine, the health authority said.
How to stay safe
Residents of the Downtown Eastside have a number of solutions they’d like to see implemented to help them stay safe.
Everyone The Tyee spoke with said they wanted to be able to access a regulated supply of drugs so they could know the potency and type of substance they were going to use.
They also wanted to see drug testing services available on every street corner. When The Tyee noted that Minister Whiteside says B.C.’s strategy is to combine drug checking services with wraparound services, William Bernier shook his head.
“Why wait? Why not put drug checking services on every corner today and then add the other services whenever they’re ready, because people are dying today,” he said.
He understands drug testing services are available but says the services are spread out and open weird hours. These are important barriers that mean people rarely use these services, he said.
For now, he said, his safety strategy is to use with a friend.
Across the street, an Overdose Prevention Society yellow tent is set up where volunteers distribute free harm reduction supplies. Overdose rates have gone through the roof in recent years, one of them says, adding he helps reverse overdoses several times per day.
“If you’re going to bed and no one has overdosed yet, the day isn’t over,” he said.
— This story was originally published by The Tyee.
News from © iNFOnews, 2023