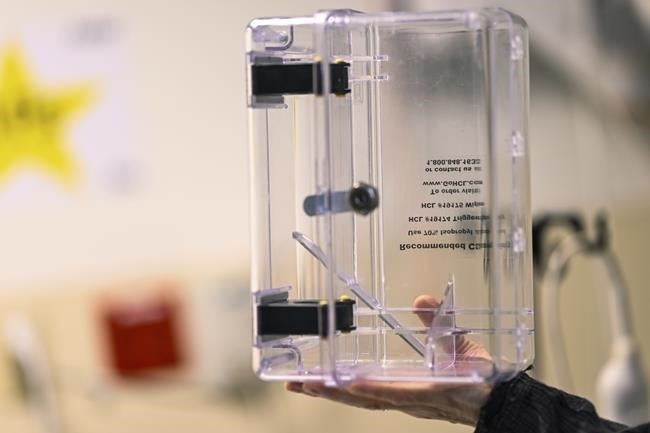
A lockbox is held to show where ketamine is placed into while administered at the Duke Speciality Infusion Center, Friday, Oct. 27, 2023, in Durham, N.C. Ketamine prescriptions have soared in recent years as an alternative to opioids for pain. But with little research on its effectiveness, some experts worry about the risks of overprescribing another powerful drug that carries risks of safety and abuse.
Image Credit: AP Photo/Matt Kelley
November 06, 2023 - 9:00 PM
WASHINGTON (AP) — As U.S. doctors scale back their use of opioid painkillers, a new option for hard-to-treat pain is taking root: ketamine, the decades-old surgical drug that is now a trendy psychedelic therapy.
Prescriptions for ketamine have soared in recent years, driven by for-profit clinics and telehealth services offering the medication as a treatment for pain, depression, anxiety and other conditions. The generic drug can be purchased cheaply and prescribed by most physicians and some nurses, regardless of their training.
With limited research on its effectiveness against pain, some experts worry the U.S. may be repeating mistakes that gave rise to the opioid crisis: overprescribing a questionable drug that carries significant safety and abuse risks.
“There’s a paucity of options for pain and so there’s a tendency to just grab the next thing that can make a difference,” said Dr. Padma Gulur, a Duke University pain specialist who is studying ketamine's use. “A medical journal will publish a few papers saying, ‘Oh, look, this is doing good things,’ and then there’s rampant off-label use, without necessarily the science behind it.”
When Gulur and her colleagues tracked 300 patients receiving ketamine at Duke, more than a third of them reported significant side effects that required professional attention, such as hallucinations, troubling thoughts and visual disturbances.
Ketamine also didn't result in lower rates of opioid prescribing in the months following treatment, a common goal of therapy, according to Gulur. Her research is under review for medical journal publication.
PSYCHEDELIC EXPERIENCE
Ketamine was approved more than 50 years ago as a powerful anesthetic for patients undergoing surgery. At lower doses, it can produce psychedelic, out-of-body experiences, which made it a popular club drug in the 1990s. With its recent adoption for pain, patients are increasingly encountering those same effects.
Daniel Bass, of Southgate, Kentucky, found the visual disturbances “horrifying.” His doctors prescribed four- to six-hour IV infusions of ketamine for pain related to a rare bone and joint disorder. Seated in a bare hospital room with no stimulation or guidance on the drug's psychological effects, Bass says he felt "like a lab rat.”
Still, he credits ketamine with reducing his pain during the year that he received twice-a-month infusions.
“No matter how horrific an experience is, if it allows me to be more functional, I will do it,” Bass said.
Ketamine targets a brain chemical messenger called glutamate, which is thought to play a role in both pain and depression. It’s unclear whether the psychedelic experience is part of the drug's therapeutic effect, though some practitioners consider it essential.
“We want patients to disassociate or feel separate from their pain, depression or anxiety,” said Dr. David Mahjoubi, owner of Ketamine Healing Clinic in Los Angeles. “If they feel like they’re just sitting in the chair the whole time, we actually give them more.”
Mahjoubi’s practice is typical of the burgeoning industry: He offers IV ketamine for alcohol addiction, chronic pain, anxiety and post-traumatic stress disorder. The ketamine doses for those indications are well below those used for surgery, but Mahjoubi favors higher doses for pain than for psychiatric conditions.
Patients pay cash because most insurers don’t cover non-surgical uses of ketamine, none of which are approved by the Food and Drug Administration. Mahjoubi’s background is in anesthesiology, not psychiatry or addiction.
Patients can pay extra for ketamine nasal sprays and tablets to use between infusions. Those formulations are also not FDA approved and are compounded by specialty pharmacies.
Sending ketamine through the mail has become its own profitable business for telehealth services, such as MindBloom, which jumped into the space after regulators relaxed online prescribing rules during COVID-19.
Pain specialists who study ketamine say there’s little evidence for those versions.
“The literature for the nasal and oral formulations is pretty scant,” said Dr. Eric Schwenk of Thomas Jefferson University. “There’s just not a lot of good evidence to guide you.”
Demand for ketamine has sent prescriptions soaring more than 500% since 2017, according to Epic Research, which analyzed the trend using a database of more than 125 million patients. In each year, pain was the No. 1 condition for which ketamine was prescribed, though depression has been rising quickly.
The prescribing boom has led to shortages of manufactured ketamine, driving up sales of compounded versions.
There is more evidence for ketamine’s use against depression than for pain. In 2019, the FDA approved a ketamine-related chemical developed by Johnson & Johnson for severe depression. The drug, Spravato, is subject to strict FDA safety rules on where and how it can be administered by doctors.
Guidelines from pain societies note some evidence for ketamine’s use in complex regional pain, a chronic condition that usually affects the limbs. But the experts found “weak or no evidence” for ketamine in many more conditions, including back pain, migraines, fibromyalgia and cancer pain.
THE ‘WILD WEST’ OF KETAMINE PRESCRIBING
While the science behind ketamine is murky, the business model is clear: Physicians can purchase ketamine for less than $100 a vial and charge $500 to $1,500 per infusion.
The recent boom has been fueled, in part, by venture capital investors. Another set of consulting businesses offer to help doctors set up new clinics.
A blog post from one, Ketamine Startup, lists “Five reasons you should open a ketamine clinic,” including: “You want to be your own boss” and “You want to take control of your money-making ability.”
The clinics are facing increasing competition from telehealth services like MindBloom and Joyous, which connect potential patients with physicians who can prescribe ketamine remotely and send it through the mail.
In May, federal regulators were scheduled to roll back the COVID-era policy that allowed online prescribing of high-risk drugs like ketamine and opioids. But the Drug Enforcement Administration, facing backlash for telehealth companies and physicians, agreed to extend the flexible approach through 2024.
The current landscape is a “wild west,” said Dr. Samuel Wilkinson, a Yale University psychiatrist who prescribes both Spravato and ketamine for depression. U.S. physicians have “quite a bit of latitude” to prescribe drugs for unapproved, or off-label, uses.
“There’s good things about that and not-so-good things about that,” he said.
When used at high doses, ketamine can cause bladder damage, sometimes seen in people who use the drug recreationally. Far less is known about the neurological effects of long-term use. Ketamine was linked to brain abnormalities in rat studies, FDA regulators note.
Last month, the FDA warned doctors and patients against compounded versions of ketamine, including lozenges and pills, saying the agency does not regulate their contents and cannot assure their safety. The warning followed a similar advisory last year about nasal spray versions of ketamine.
But most compounding pharmacies are small operations, overseen by state officials, not the FDA.
In April, Massachusetts’ board of pharmacy flagged the FDA’s warning to local pharmacies, but noted that state officials wouldn't take any steps to stop “the continued compounding and dispensing of ketamine nasal spray.”
The FDA likewise has little leverage over physicians promoting ketamine, even those making exaggerated or misleading claims.
Drugmakers are subject to strict FDA regulation in how they promote their medicines — with requirements to balance risk and benefit information. Those rules don’t apply to physicians.
Even when the FDA has tried to regulate risky in-office procedures, such as unproven stem cell infusions, the agency has had a mixed track record of prevailing in court.
For now, experts say it’s unlikely regulators will go beyond their recent warnings about off-label ketamine.
“There’s an element of whack-a-mole and it’s essentially beyond their regulatory purview,” said Dr. Caleb Alexander, a drug safety researcher at Johns Hopkins University. “These clinics would represent yet another front that they would be hard pressed to manage and address.”
___
Follow Matthew Perrone on Twitter: @AP_FDAwriter
___
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.
News from © The Associated Press, 2023