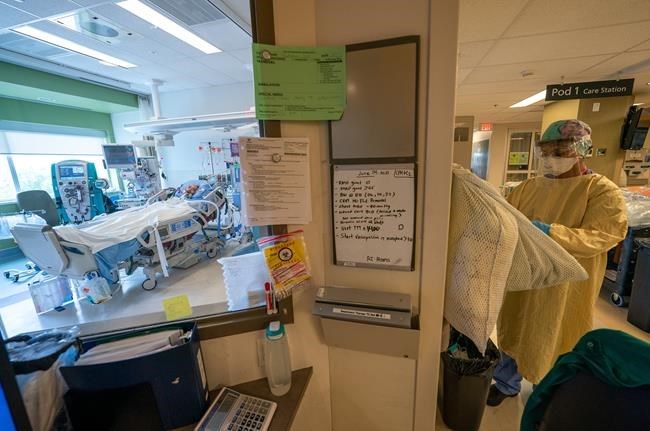
Registered Nurse Manjot Kaur Munday, prepares with her PPE prior to visiting COVID-19 patient Joseph Trudeau, 49, of Surrey, B.C. at the COVID-19 Intensive Care Unit at Surrey Memorial Hospital in Surrey, B.C., Friday, June 4, 2021. THE CANADIAN PRESS/Jonathan Hayward
November 06, 2022 - 1:00 AM
VANCOUVER - A family doctor who works in British Columbia and Alberta says patients who don't get the care they need before ending up in overburdened emergency rooms should be a focus for quick action by the country's health ministers as they meet in Vancouver.
Dr. Carllin Man said sicker patients without a family physician tend to return to ERs where burnt-out doctors and nurses put in longer and longer hours as colleagues leave the profession.
"For a long time, our health systems have relied on our goodwill as health-care professionals," Man said. "We're doing more and more when we should have stopped a long time ago, but there's no one else. What are you going to do, just let those patients suffer? Of course not."
Man, who works part-time at a walk-in clinic in Burnaby, B.C., as well as in emergency rooms in central Alberta, said he will need to refill some patients' prescriptions during an upcoming 10-day vacation because there won't be anyone to cover for him.
"So, every day I have to log into my computer and try to manage the things I can while I'm away," he said of his chronically ill patients who are not best suited for care by other doctors without full knowledge of their medical history.
Man said it's time that governments across Canada listened to the concerns of patients and those who look after them.
Health ministers from all 13 provinces and territories, along with their federal counterpart, Jean-Yves Duclos, are set to meet in Vancouver on Monday and Tuesday.
The meetings come four months after premiers from across Canada convened in Victoria to discuss the ills plaguing the health-care system. The premiers asked the federal government to hike the Canada Health Transfer, the money each jurisdiction gets for health care, to 35 per cent, from 22 per cent.
B.C. Health Minister Adrian Dix said the extra cash is needed as the province tackles nursing and doctor shortages, improved access to digital health care, as well as mental health and substance-use services related to the toxic drug crisis.
"We need the federal government to be our partner in this approach," he said in a statement. "That means having a serious discussion about the Canada Health Transfer."
The Canadian Medical Association, the Canadian Nurses Association and HealthCareCAN, which represents various organizations and hospitals, have joined forces to push the health ministers to retain workers through incentives like mental health supports.
They are also calling for a Canada-wide strategy to gather data on the workforce, allow doctors to more easily be licensed wherever in the country they are most needed, and to improve access to primary care and virtual visits.
Man completed his training in Alberta seven years ago but said getting his licence to practise in British Columbia was a months-long, arduous process.
"I had to jump through all these hoops. I had to physically travel to Vancouver, to the (College of Physicians and Surgeons' office), to show my face and my degrees. I mean, they didn't do that in Alberta. They trusted the fact that I was licensed with the National Medical Council of Canada and all these other national organizations that verify our educational degrees and training."
Dr. Alika Lafontaine, president of the Canadian Medical Association, said the collapse of primary care is spilling into other parts of hospitals beyond ERs, as well as long-term care, due to cost-cutting.
"There's a recognition that we have fallen far behind the demand for health services in every part of the country. In Ontario, there are tens of millions of health services and thousands of surgeries that have been delayed," said Lafontaine, who is an anesthesiologist in Grande Prairie, Alta.
"The biggest fear that I have for the health-care system moving forward is that those of us who believe it will be there tomorrow, it may not actually be there in the same form. And you won't actually know that until you need the care."
Lafontaine said he is hoping the meeting of health ministers results in collaboration across Canada "because the crises are too big for any one jurisdiction. If we don't act, all of our systems will continue to deteriorate. And I think the impetus for action is now because of how severely patients are suffering."
Sylvain Brousseau, president of the Canadian Nurses Association, said undervalued nurses are leaving their jobs because their mental health is suffering due to poor working conditions.
He said they are often tasked with work that has nothing to do with their training, due to lack of clerical and cleaning staff.
"Nurses are doing 48 per cent of non-nursing duties," he said.
"When you ask a nurse to clean the floor because someone has been sick, it's not the role of nurses to do that."
Brousseau said the time for ongoing discussions by federal, provincial and territorial politicians when it comes to resourcing health care is over.
"We've dialogued a lot. Now, it's time for action," he said. "No nurses, no health-care system."
This report by The Canadian Press was first published Nov. 6, 2022.
News from © The Canadian Press, 2022